This story has been nearly thirty years in the making. The timing never quite felt right as I always had hope that better things were to come. Fortunately, this optimism has paid off and I have recognized what was holding me back from starting writing.
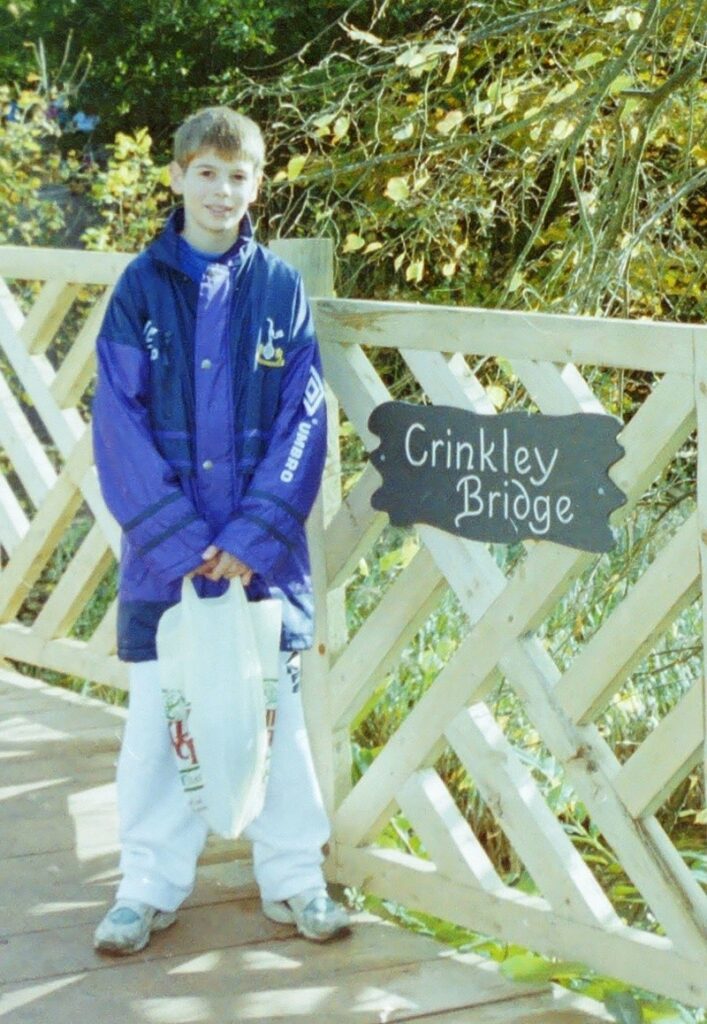
My pituitary story started in the spring of 1995, when I was 14. I first remember struggling with two things: reading became a problem, with the tops and tails of the characters becoming indistinguishable, meaning d, g, a and q all looked the same; and my colour vision deteriorated. This progressed over a few months with my vision deteriorating further with permanent “floaters”, like when you look at a bright light and best described as black holes in my vision. Over the months these became both more numerous and bigger, meaning I was down to around 30% vision.
The optician noticed issues with the blood vessels at the back of my eyes and referred me to the GP for a diabetes test, which was negative. I was then referred to a community ophthalmologist, who told my mother I was attention seeking and not to pander to me! Luckily, he did refer me to a specialist at Moorfield’s Eye Hospital, and I was fortunate enough to be looked after by Mr Riordan-Eva, who pretty much diagnosed me immediately. He was amazing, spending his entire morning clinic with me, listening to my symptoms, running tests, taking bloods and arranging follow up tests, the first of which was a CT scan.
The other tests proved unnecessary. The CT scan showed a craniopharyngioma and I was immediately introduced to Mr Hayward, who was now my consultant paediatric neurosurgeon. The next five days were a whirlwind, with an MRI scan scheduled to assist with surgery and admission to Great Ormond Street Hospital for a craniotomy.
Looking back in hindsight there were other obvious symptoms too. The debilitating headaches (put down to migraine), slowed growth (a late developer) and frequent passing of urine being some others.

The surgery went better than expected and afterwards I didn’t even realise I had come out of surgery. Except there was one thing that was different. What was it? I couldn’t quite pin it down. Then three days later I realised, with the words that will live with me forever: “Mum, I can see! I can read the nurse’s name badge. Susan Joyce, Staff Nurse”. The relief is impossible to put into words!
This pre-internet-era-naivety was both a blessing and a curse! I think it was natural to think “right, well that’s done, I was lucky, phew, onwards and upwards”. Sadly, that was not to be. A nasty chest infection in hospital was the first rude awakening, setting me back in my recovery. Then there was the small matter of my entire pituitary gland being removed in the operation. Can’t be that important can it?
Turns out the little pea sized gland behind your eyes is vital! Learning new terms and medicine names was overwhelming at first (thank you to The Pituitary Foundation for being by side throughout!), but soon becomes second nature and I now consider myself a patient expert. I am on the full set of replacement meds: hydrocortisone, desmopressin, thyroxine, growth hormone, testosterone and vitamin D.
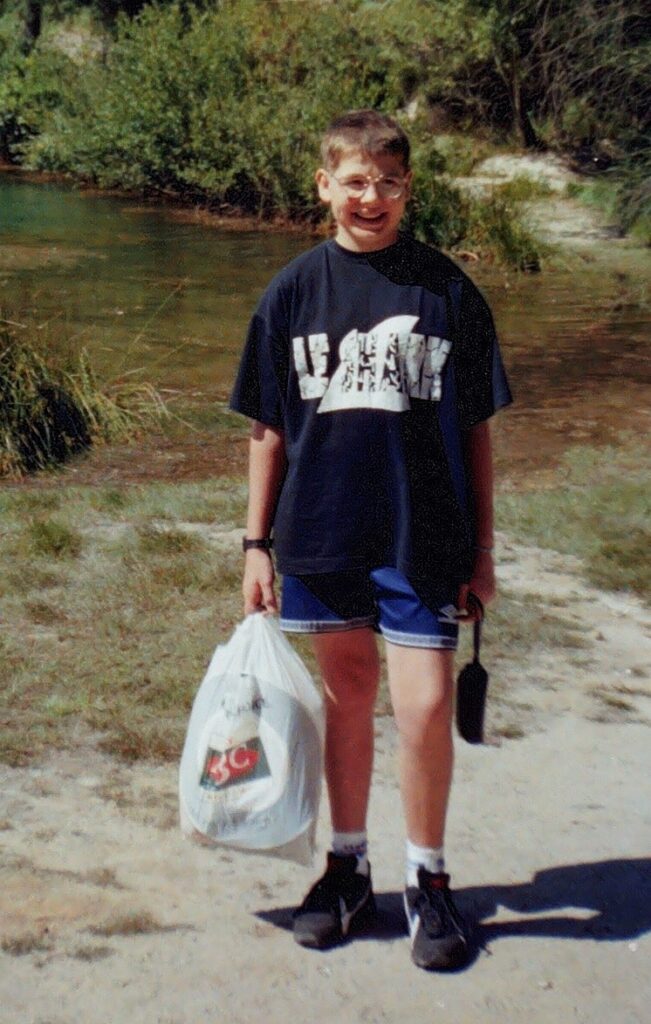
I am able to say I have been very lucky! Despite a year of building up my strength and attending school perhaps ten times for an hour or two at a time in the first year of my GCSEs, I was able to catchup and get great results, moved on to A levels and got a degree in Economics at University College London (next door to my Consultant Endocrinologist, which was handy!).
It wasn’t all plain sailing however. Stopping growth hormone, aged 19, in the first year of my degree left me bedridden and I nearly failed the first year of my degree as I could barely make it to my exams. Luckily with support from my Endocrinologist I was soon back on the GH and back on track and graduated with a first class honours. Since then I have qualified as an accountant and work full-time in Finance.
There have been ups and downs since. Often it takes a while to adjust to changes in my medications and doses. Things have fortunately come a long way in the time I have been a patient. No more having to carry a cool bag with me everywhere I go and worrying about how my DDAVP will absorb as I have yet another blocked nose from taking a nasal spray three or four times a day!
However, the biggest progress has by far been in the psychological space. At the time of my treatment in 1995 there was precious little support in this regard. I went through the years afterwards feeling generally lucky to be where I was (the waiting room in GOSH is a great place to get perspective!). I couldn’t really understand why over time I felt increasingly numb and like I had lost my spark.
Then 22 years after my operation I had the breakthrough (unfortunately via a breakdown). To cut a long story short, diagnoses and treatment for depression, anxiety, perfectionism, low self-esteem and low assertiveness amongst others led to the underlying cause. I had PTSD.
That made so much sense and after several years of on and off treatment I am now in a far better place. My brain is continuing to readjust after so many years of living in fight or flight mode, and I am now feeling ready and able to share my story.
I remain optimistic about the future and it is so positive to see new developments being researched, after what has felt like a long period of stability. The two projects I am personally most excited about are the effects of oxytocin replacement and the patches to monitor cortisol levels throughout the day. I’m sure both will benefit me and many other patients in future.
My top tips are definitely keeping a sense of humour and finding your passion. For me I realise music is really important and is a good insight into how I am feeling, which allows me to respond in a positive way. Also be your own advocate when you feel you are not being listened to by doctors. It is great to know The Pituitary Foundation is also there for us when we need them.









