Adrenal Insufficiency and Adrenal Crisis
An adrenal crisis is a medical emergency. If you suspect you, or someone else, is experiencing an adrenal crisis you should call 999 and state that you / they are having an adrenal crisis.
The below information relates to adrenal insufficiency and adrenal crisis. Click here for our emergency information for AVP deficiency.
What is an adrenal crisis?
Adrenal crisis is a life-threatening situation where the level of cortisol in your body has dropped too low.
Common causes of adrenal crisis are:
- Sudden onset of diarrhoea and / or vomiting,
- A rise in body temperature to above 38 °C
- A Significant accident or injury
- Sometimes, intense psychological stress, such as bereavements or witnessing trauma, can lead to adrenal crisis
Signs of an adrenal crisis
Signs of low cortisol and adrenal crisis include:
- Headache
- Nausea
- Irritable / restless
- Clumsiness
- Fatigue
- Pale skin (if you have darker skin this may look ashen or grey)
- Muscle aches
- Weakness
- Shivery / cold
- Spasms
- Dizziness (especially on standing)
- Stomach pain / diarrhoea
- Vomiting
- Reduced / loss of consciousness
- Seizures
It’s important to note that you may not have all of these symptoms. For more information on signs of adrenal crisis, see our Adrenal Crisis Signs Table.
If you have more than one of these symptoms at the same time, your cortisol levels are likely to be too low for your current illness or stressful situation.
Similarly, if you find symptoms start to accumulate, (e.g. headache, followed by nausea, then feel shivery cold, with leg aches and fatigue) this may also indicate inadequate cortisol levels. Taking extra cortisol by mouth, as outlined in the Sick Day Rules Table, at this time can often prevent a full-blown adrenal crisis.
What to do if you’re having an adrenal crisis
If you are having an adrenal crisis you should call 999 and state that you are having an adrenal crisis / Addisonian crisis and describe the symptoms that you are experiencing (e.g. vomiting, diarrhoea, dehydration, injury/shock).
Whilst you wait for the ambulance you should administer your emergency hydrocortisone injection. If you are unsure if what you are experiencing is an adrenal crisis then you should still administer your emergency injection.
How to administer an emergency hydrocortisone injection (pre-mixed and powder)
Step 1: Ensure you have all the equipment listed. Clean the injection site (mid-upper thigh) and wash your hands if possible.
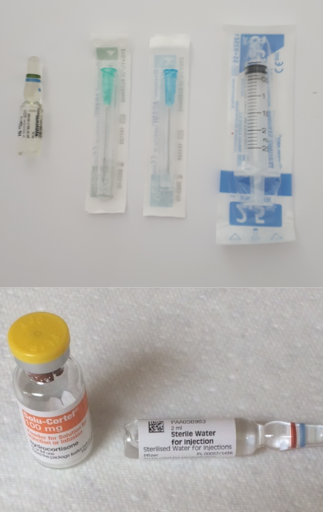
Equipment:
- 1 x drawing up needle (green)
- 1 x injection needle (blue)
- 1 x 2 ml syringe
and
- 1 x ampoule (glass bottle) of hydrocortisone (for pre-mixed solution version)
OR (for powder version)
- 1 x ampoule (glass bottle) of water
- 1 x ampoule (glass bottle) of powder
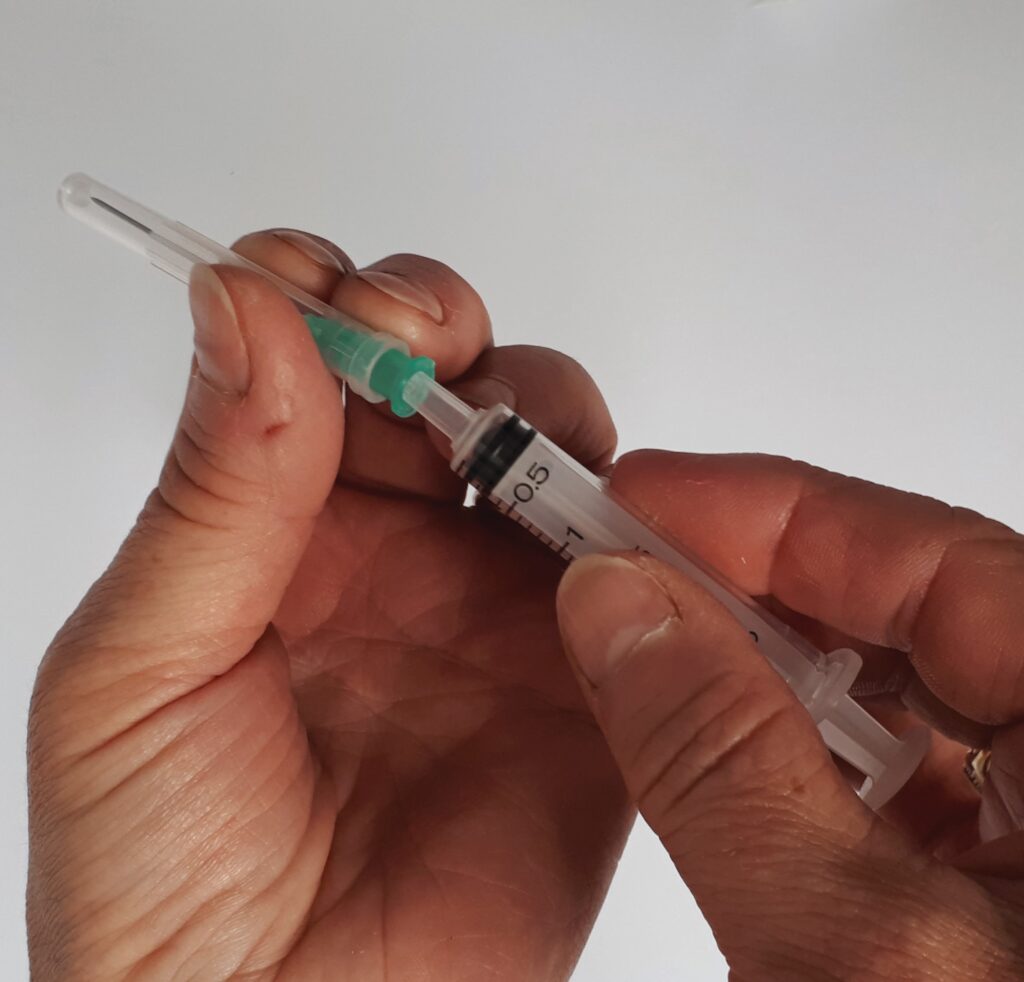
Step 2: Open the plastic packets on the needles and syringe and attach the green ‘drawing up’ needle to the syringe

Step 3: Make sure all the liquid is at the bottom of the ampoule. If using the pre-mixed version, this will be liquid hydrocortisone. If using the powder version, this will be water.
Hold the ampoule with the blue dot facing backwards. Break the top off the ampoule by ‘snapping’ the blue dot backwards. You can use a tissue to hold the ampoule to avoid cuts.

Step 4: Take the cap off the green needle. Place the tip of the needle into the open ampoule (this can be tipped without losing the liquid). Pull back the plunger to draw the liquid up into the syringe.
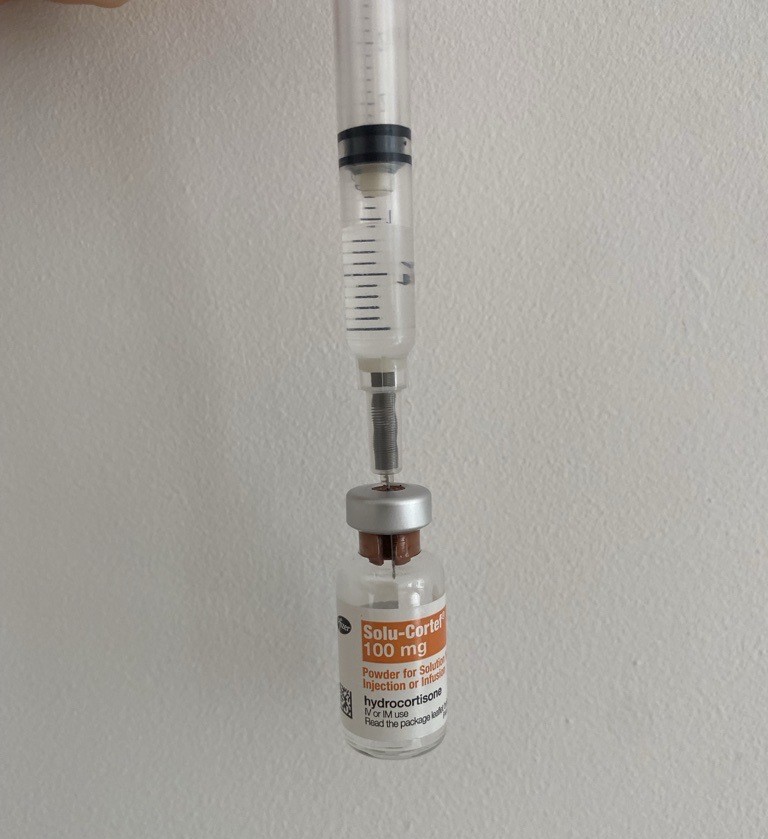
Step 5: For powder version only (if using pre-mixed solution, skip to step 6).
Hold the powder ampoule on a flat surface. Push the needle through the rubber top and push the plunger of the syringe down to inject water into the powder ampoule. Keep the plunger down and remove the needle. Mix the powder and water with a swirling motion for a few seconds. Re-insert the needle into the ampoule and draw up the mixed liquid, same as in step 4.

Step 6: Hold the filled syringe with the needle facing up. Remove the green ‘drawing up’ needle and place it in a sharps bin, if one is available. Now attach the blue ‘injection’ needle. Gently tap the syringe to make sure there are no air bubbles in the liquid. If there are air bubbles, you can push the plunger down a little bit to push them out.

Step 7: Hold the barrel of the syringe between the thumb and forefinger of your dominant hand. Take off the needle cover and use the other hand to support the skin at the injection site. Hold the needle at a 90 degree angle to the injection site. Push the needle into the skin of the mid-upper thigh, using a smooth, steady push.

Step 8: Smoothly push down the plunger until all the liquid has been injected into the leg. Carefully remove the needle and apply gentle pressure to the injection site with a cotton swab or tissue.

Step 9: Place any used equipment (including needles, syringes and ampoules) into a sharps container, if one is available. Make sure the ambulance has been called and stay with the person until they arrive.
You can also watch this video on how to administer an emergency injection.
People with adrenal insufficiency should always make sure they have an emergency hydrocortisone injection kit on their person, including when out and about, at work and on holiday. For more information on what this kit should include, see our overview of emergency hydrocortisone injection packs.
Sick Day Rules
During normal health and life, when you become ill or suffer injuries the body produces increased levels of cortisol to help us survive those stresses. Now that you are unable to produce your own cortisol, you need to be aware of when to provide an increased cortisol level during stressful times or during ill health. The amount of increase needed, the way the cortisol is given and the length of time the increase is needed will vary depending on the situation you are in.
Following the Sick Day Rules is important to prevent adrenal crisis. If you do not take enough cortisol in response to stress or illness, you may progress to an adrenal crisis.

Download our Sick Day Rules Table
You can download this table of the steroid Sick Day Rules, to take with you on the go
Download nowAVP Deficiency (Diabetes Insipidus)
The following provides emergency information relating to AVP deficiency.
Sick Day Rules
You can download our Desmopressin Sick Day Rules table, which covers illness and emergency situations for people taking desmopressin.
You should seek medical attention if any of the following happen:
- You have missed or cannot take your desmopressin and have little or no access to fluids
- You have taken your desmopressin as normal but have then had a large intake of fluid
- You have vomiting (more than once) and / or diarrhoea
Your healthcare team should seek advice from an endocrinologist experienced in AVP-D (DI).
You may want to share this link to the Society for Endocrinology Emergency Care Guidance for the Emergency Management of Severe Symptomatic Hyponatraemia in Adult Patients with your clinician.
See below for more information on possible emergency situations.
AVP-D emergency situations
Why is this a problem?
By not taking desmopressin, your body will not be able to control urine output. This means you will continue to lose water. If you are not able to replace this lost water through drinking this can lead to dehydration and increased levels of sodium in the blood. An increase in sodium in the blood is known as hypernatraemia.
Why is hypernatraemia an emergency?
High sodium is very uncommon unless the body is severely lacking in water. If this is not recognised and treated, it can be life-threatening as it can cause problems with the brain and central nervous system. If you have AVP-D (DI), not taking desmopressin can lead to hypernatraemia if you also doesn’t have access to fluids to replace lost water.
Hypernatraemia can also develop if you have an episode of gastroenteritis (stomach flu) or repeated vomiting, due to increased fluid loss caused by vomiting and/or diarrhoea. Correcting a too-high sodium level should be done carefully to prevent too sudden a drop.
What symptoms might I have?
Symptoms of a high sodium can include:
- Headaches
- Fatigue or tiredness
- Irritability
- Dry mouth and lips
- Nausea and reduced appetite
- Cramps
- Muscle spasms
- If left untreated, sometimes convulsions or seizures may occur
Seeking help
-
- Attend your GP without delay if early symptoms of headache, tiredness and irritability
-
- Attend A&E if have early symptoms and nausea, low appetite, cramps, muscle spasm
-
- Call 999 if convulsion or seizures occur
Why is this a problem?
This mean you will may have too much fluid in your system, as you will have reduced your urine output with the desmopressin. Having a high fluid intake after taking your desmopressin can lead to a reduced blood sodium level, known as hyponatraemia. This can lead to seizures.
Hyponatraemia (low sodium) can be graded as mild, moderate or severe. Correcting hyponatraemia has to be done very carefully to prevent too sudden a rise in blood sodium. The level of emergency medical attention needed will depend not only on your sodium levels but also on your symptoms at the time.
How does this cause hyponatraemia?
When you take desmopressin this signals to your kidneys to hold onto the water in your blood, meaning less water is lost as urine. Too high a dose or too much of desmopressin can cause too much water to be kept in the body and this can lower your blood sodium levels. If you continue to have a strong thirst, and drink to quench the thirst after taking desmopressin, this can also cause over-dilution of the blood and so lower your blood sodium levels.
Other illnesses can also cause a shift in your fluid balance and result in a drop in sodium levels, especially if you have vomiting and / or diarrhoea.
What symptoms might I have?
Symptoms can vary and do not always match the level of blood sodium in their severity. If you have mild or moderately low blood sodium you may still have severe symptoms.
Moderate symptoms include:
- Nausea without vomiting
- Confusion
- Headaches
Severe symptoms include:
- Vomiting
- Seizures
- Reduced level of consciousness and possibly cardiac arrest
Seeking help
If you have any of these symptoms listed above you should seek emergency medical attention.
Why is this a problem?
This will affect your fluid balance levels and the levels of sodium and potassium in your blood. It may become difficult for you to keep control of your AVP-D (DI). This is especially important if you take cortisol replacement, as reduced cortisol levels also have an impact on your blood sodium levels. This situation would need you to attend accident and emergency or an urgent care department for urgent assessment and stabilisation.
If you have taken extra desmopressin for whatever reason and your urine output has dropped significantly, as long as you are not thirsty and dehydrated, try to limit your fluid intake and take no further desmopressin until you have symptoms of thirst and an increasing urine output. If your urine output does not increase within 12 hours then seek medical advice.